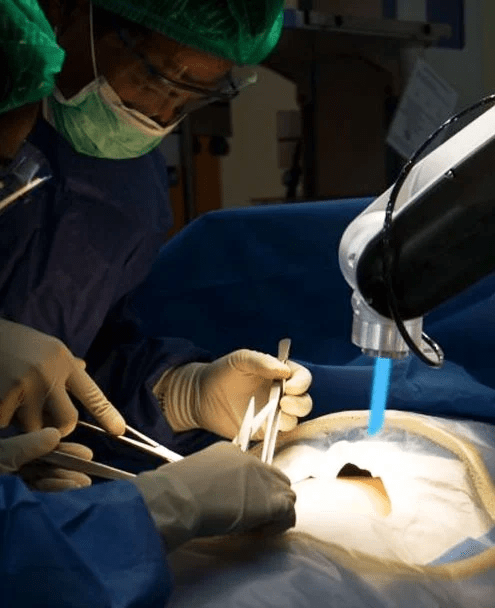
Medical Arts Surgical Group Robotic Hiatal Hernia Surgeon
Hiatal Hernia and GERD
The presence of a hiatal hernia is identified when some of the stomach moves through the diaphragm, reaching the chest cavity. The diaphragm, which acts as the muscular boundary between the chest and abdominal areas, is indispensable for breathing functions. This arrangement can be compromised by a hernia, augmenting the probability of acid reflux into the esophagus, potentially instigating gastroesophageal reflux disease (GERD). GERD denotes a chronic state where there's a regular reflux of stomach acid into the esophagus, causing symptoms such as heartburn, reverse flow of stomach contents, and at times, issues with swallowing. Continuous GERD can culminate in complications like esophageal soreness, constrictions in the esophagus, or the occurrence of Barrett's esophagus.
Medical Arts Surgical Group Robotic Hiatal Hernia SurgeonMedical Arts Surgical Group Robotic Hiatal Hernia Surgeon